Introduction
Enzyme-linked immunosorbent assays (ELISAs) are widely used diagnostic techniques due to their versatility, sensitivity, and relative ease of use. This blog post explores the fundamental principles of ELISAs and their application in diagnosing various common diseases.
Core Principles of ELISA
An ELISA relies on the specific binding between antigens and antibodies. Here's a breakdown of the key steps:
- Antigen Coating: A microplate is coated with a specific antigen that binds the target molecule (e.g., pathogen antigen, hormone) from the patient sample.
- Sample Introduction: The patient's serum or plasma is added to the plate. If the target molecule is present, it binds to the coated antigen.
- Washing: Unbound components are removed using a washing buffer.
- Detection Antibody Addition: A detector antibody conjugated to an enzyme (often horseradish peroxidase - HRP) is introduced. This antibody specifically binds to the target molecule captured in step 2.
- Washing: Unbound detection antibodies are eliminated with another washing step.
- Substrate Addition and Signal Generation: A substrate specific to the HRP enzyme is introduced. The HRP catalyzes a reaction, generating a measurable signal (color change, luminescence) proportional to the amount of target molecule present in the sample.
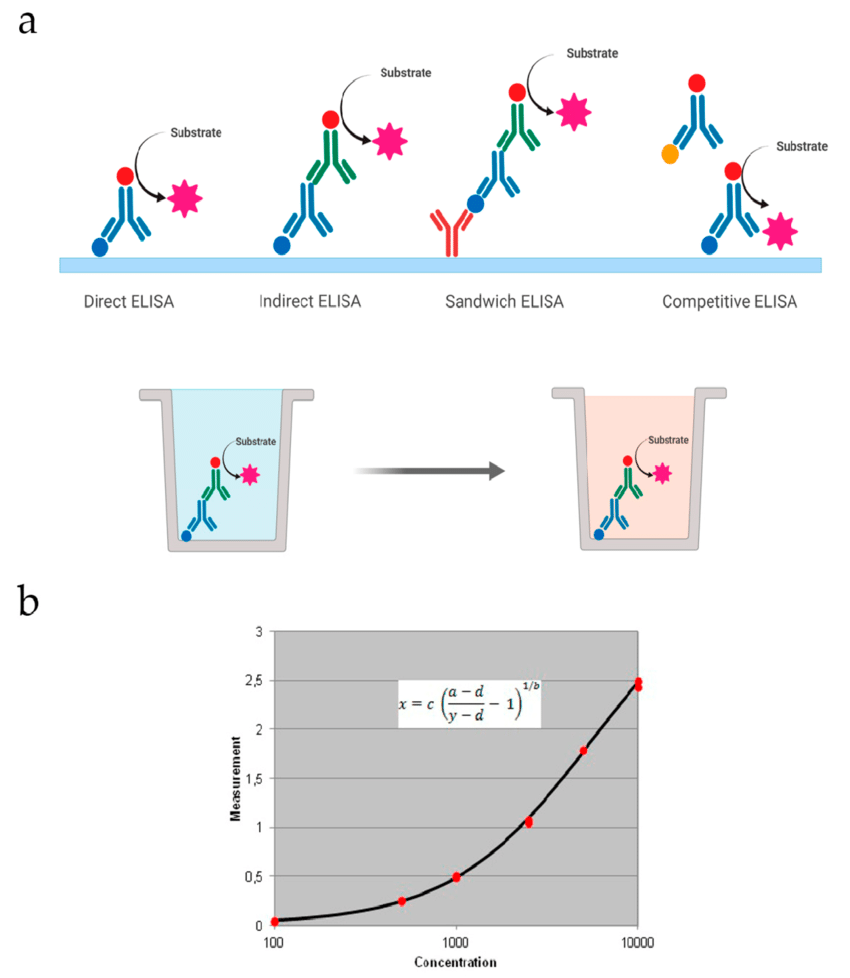
ELISA Variations for Diverse Applications
Several ELISA formats cater to specific needs:
- Direct ELISA: Uses a primary antibody directly conjugated to the enzyme (simpler but potentially less sensitive).
- Indirect ELISA: The most common format, employing a secondary detection antibody conjugated to the enzyme for increased sensitivity.
- Sandwich ELISA: Utilizes two capture antibodies targeting different regions of the target molecule for enhanced specificity.
- Competitive ELISA: The sample competes with a known amount of labeled antigen for binding sites, useful for quantifying small molecules.
ELISA Applications in Common Disease Diagnosis
ELISAs play a crucial role in diagnosing various diseases, including:
- Infectious Diseases: Detect antibodies against viral (HIV, Hepatitis C) or bacterial (Lyme disease) antigens for diagnosis and treatment monitoring.
- Autoimmune Diseases: Identify autoantibodies directed against self-tissues, aiding in diagnosing rheumatoid arthritis, systemic lupus erythematosus, etc.
- Allergic Disorders: Detect allergen-specific IgE antibodies to diagnose allergies.
- Hormonal Imbalances: Measure hormone levels (thyroid hormones, insulin) to diagnose endocrine disorders.
Advantages and Limitations of ELISAs
Advantages:
- High Sensitivity: Can detect very small amounts of target molecules.
- Specificity: Tailored antibodies ensure specific detection of the target molecule.
- Versatility: Adaptable to various analytes and formats.
- Ease of Use: Standardized protocols facilitate widespread application.
- Cost-Effectiveness: Amenable to high-throughput testing.
Limitations:
- Potential for Errors: Factors like cross-reactivity or suboptimal test conditions can affect accuracy and lead to false positive/negative results.
- Limited Information on Disease Activity: May not always distinguish between active and past infection or disease.
- Specialized Equipment and Expertise: Proper training and infrastructure are necessary for reliable results.
Conclusion
ELISAs are powerful and adaptable tools for researchers and clinicians in diagnosing various common diseases. Understanding their core principles and diverse applications is essential for developing novel assays and interpreting test results effectively. However, it's crucial to acknowledge the limitations associated with ELISAs, such as the need for specialized equipment and expertise. For labs lacking in-house resources,
Suppliers like Gentaur
can offer a valuable alternative, providing standardized protocols and pre-measured reagents. Nevertheless, integrating ELISAs with other diagnostic tools remains essential for a comprehensive patient evaluation.